Releasing more stem cells.
Recently I had the privilege of interviewing world renown Stem Cell expert Dr Christian Drapeau on my podcast "Pushing the Limits"
Dr Drapeau has spent over 2 decades studying stem cells in the body and how to mobilise more from the bone marrow into circulation and into the tissues.
Here an article by Dr Drapeau
ENDOGENOUS STEM CELL MOBILIsATION A NEW PARADIGM
INTRODUCTION
Over the past decade the world has seen an unprecedented explosion in the field of stem cell research.
Hardly a week passes by without an article in one of the main printed newspapers, describing a new breakthrough involving stem cells.
Stem cell research is arguably today one of the most prolific fields of science. And yet, little of the available information has reached the general population – or even the health profession – in a manner that allows people to clearly understand the basics as well as the tremendous promise of stem cell research.
And at the center of all this development in stem cell research is a fundamental question that is rarely talked about: if adult stem cells hold such a potential for tissue repair and regeneration, what about the stem cells naturally present in the bloodstream and the bone marrow?
If isolating stem cells from the bone marrow and then reinjecting them in the bloodstream can hold such a potential for health, what about simply supporting the natural release of the stem cells already present in the bone marrow?
What is the natural role of the stem cells normally present in the body?
This line of study has led to what is referred to as Endogenous Stem Cell Mobilisation: the release of your own stem cells.
The purpose of this article is to describe the therapeutic potential of this approach. WHAT IS A STEM CELL?
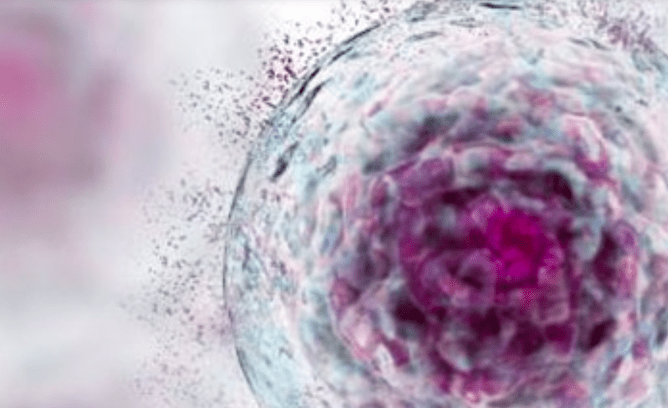
Stem cells are defined as cells with the unique capacity to self-replicate throughout the entire life of an organism and to differentiate into cells of various tissues.
Most cells of the body are specialised and play a well-defined role in the body.
For example, brain cells respond to electrical signals from other brain cells through the release of neurotransmitters, cells of the retina are activated by light and pancreatic ß-cells produce insulin.
These cells, called somatic cells, will never differentiate into other types of cells or even proliferate. By contrast, stem cells are primitive cells that remain undifferentiated until they receive a signal prompting them to become various types of specialized cells.
Generally speaking, there are two types of stem cells: embryonic stem cells and adult stem cells. Embryonic stem cells (ESC ) are cells extracted from the blastula, the very early embryo, while adult stem cells (ASC) are stem cells found in the body after birth.
The term “adult stem cells” does not refer to characteristics associated with adulthood. Stem cells in the bone marrow of a newborn, for example, or even stem cells found in the umbilical cord are referred to as adult stem cells. Scientific Bias Against Adult Stem Cells The manner with which stem cells have been defined has created a significant bias that has hindered the development of adult stem cell research for a long time.
Through the course of scientific investigations, ESC became defined as cells having the ability to grow many generations in vitro, to maintain their integrity after many generations, to become cells of virtually any tissue of the body and to form a teratoma (a tumor) when injected in the body. Initially this concept was meant to define all stem cells.
However, at the time, when these methods were used to investigate ASC, they were found to be very difficult to grow in vitro, they did not maintain their integrity after many generations in vitro, they did not differentiate easily in vitro, and injection of ASC did not lead to the formation of a teratoma.
Therefore, for a long-time ASC were considered lesser stem cells with very little capability and therapeutic potential. ASC certainly showed some level of “stemness”, as evidenced by the ability of hematopoietic stem cells or blood adult stem cells to become red blood cells, lymphocytes and platelets, but the belief that they were limited in their ability to become other types of cells led to a general lack of investigation of their therapeutic potential.
They were simply considered lesser stem cells. However, the potential of ASC has been clearly revealed over the past 15 years thanks to the work of numerous scientific teams throughout the world. A large body of scientific data indicates that ASC have capabilities comparable to ESC when studied in a living organism as opposed to a test tube.
For example, an ASC exposed to brain tissue will rapidly become a neuron or a glial cell,1,2 when exposed to liver tissue ASC will rapidly become liver cells,3,4 and hair follicle stem cells can regenerate a sectioned spinal cord.5
In short, ASC can virtually become every cell type of the body, opening an entirely new path of research in the field of health and wellness.
The Potential of Adult Stem Cells
Today we know that ASC are undifferentiated or primitive cells that can self-renew and can differentiate into specialised cells of various tissues.
Though ASC are most predominantly found in the bone marrow, they can also be isolated from various tissues such as the liver,12 the intestine,13 muscles,14 the brain,15 the pancreas,16 as well as blood and many other tissues.17
The role of ASC found in tissues is to maintain and repair the tissue in which they are found, though local stem cells appear to be involved only in relatively minor repair of the tissue in which they reside. In case of major injury or degeneration, the need for stem cells far exceeds the number of stem cells available in the tissue, and stem cells from the bone marrow (BMSC) are called to contribute to the repair process. BMSC have traditionally been considered to have little potential for plasticity, being limited in their development to red blood cells, lymphocytes, platelets, bone and connective tissue.
However much scientific work has been published over the past decade demonstrating the exceptional plasticity of BMSC. After transplantation, bone marrow and enriched hematopoietic stem cells (HSC) were shown to have the ability to become muscle cells, heart cells,endothelium capillary cells, liver cells, lung, gut and skin cells,as well as neural cells.
THE STEM CELL SYSTEM OF REPAIR
As mentioned previously, ASC are well known for their role in the constant renewal of blood cells (red blood cells, lymphocytes and platelets) and the regeneration of bone, ligament, tendon and connective tissues. But until recently it was believed that this was the extent of their ability to become other types of cell. So how was the true role of stem cells in the body discovered?
How is it that with today’s level of scientific sophistication, we only recently discovered this phenomenon? Because if we think about it carefully, such a discovery amounts to nothing less than the discovery of a whole new system in the body!
A system is a tissue or organ or a set of tissues and organs comprised of specific cells that accomplish specific tasks affecting other organs and tissues, aimed at supporting the health and survival of the whole organism.
For example, the cardiovascular system is comprised of the heart and its task is to pump blood in order to deliver nutrients and oxygen to every cell of the body. The digestive system is comprised of the stomach and intestine and its task is to digest food into absorbable nutrients in order to feed every cell of the body.
The endocrine system is comprised of several organs whose task is to secrete compounds called hormones that modulate the functioning of other organs and tissues.
For example, the pancreas secretes insulin that allows the transport of glucose into cells, and the thyroid gland secretes thyroid hormones that stimulate body metabolism. Regarding stem cells, we have the bone marrow that secretes CD34+ cells that travel and migrate into damaged tissues, restoring optimal functioning. Science has discovered the repair system of the body!
How can such a discovery have waited so long to be made?
We can find the answer in the history of science itself, where oftentimes breakthrough discoveries are only made once the necessary tools have been developed. For example, how did we discover bacteria? After the development of the microscope. The microscope was originally developed to count thread density in fabrics.
One day, pushed by curiosity, Antonie van Leeuwenhoek used his microscope to look at a drop of water and described for the first time tiny microorganisms moving in the water. Bacteria were observed for the first time… and not only were bacteria thus discovered, but we soon realized that bacteria are everywhere to be found.
The discovery of the role of stem cells in the body follows the same storyline. A spontaneously fluorescent protein called green fluorescent protein (GFP) was isolated from the jellyfish Aequorea victoria.
Since GFP is a protein, it is possible to derive the DNA responsible for its production and to incorporate the GFP-gene in the nucleus of a stem cell. In such case, all the cells derived from the original fluorescent stem cell will be fluorescent.
The discovery of GFP is of such importance that it was awarded the 2008 Nobel Prize in chemistry. When scientist began injecting fluorescent stem cells in irradiated animals –a treatment that kills all stem cells in the body–, soon thereafter fluorescent tissue cells began to appear in various tissues.
But more importantly, if any specific tissue was injured or damaged, the area of the injury would soon begin to display significant amounts of fluorescence. The injured area was being filled with new functional specialized cells of that tissue, but the cells were fluorescent, indicating that they came from the bone marrow.
A process that until then had been virtually invisible suddenly became visible – a discovery that is changing the very way in which we view biological science!
Thanks to the discovery of GFP, adult stem cells from the bone marrow have been shown to have the ability to naturally become, in the body, cells of the liver, muscle, retina, kidney, pancreas, lung, skin and even the brain … putting an end to the dogma that we are born with a set number of brain cells and that the brain cannot regenerate.
But the most fascinating observation emerging from these studies is that this process is natural. After an injury or a simple stress in an organ, bone marrow stem cells travel to that organ and play a crucial role in the process of tissue repair.
The Stem Cell System of Repair Have you ever wondered what happens when you cut or burn your skin or break a bone?
How does the body repair itself? The conventional view is that skin cells called fibroblasts create an extracellular matrix made of collagen, on which epithelial cells proliferate and migrate to reconstitute the damaged tissue. Although this process appears to explain the phenomenon of repair in small superficial injuries, it cannot account for the repair of more significant tissue damage.
First, epithelial cells do not have the ability to differentiate into all the various cell types involved in the repair of complex tissues.
For example, when considering skin repair, the newly formed skin will contain hair follicles, sebaceous glands, and sweat glands, and epithelial cells do not have the ability to become such cells.
And second, epithelial cells or other cell types generally do not proliferate at a rate that can account for the rapid repair process taking place in various tissues.
What has emerged over the past few years, through a vast body of scientific literature, is the novel view that the process of repair and renewal taking place in the body involves bone marrow stem cells. In brief, when a tissue is subjected to significant stress, stem cells originating from the bone marrow migrate to the tissue, proliferate and differentiate into cells of that tissue, thereby supporting the repair process.24
This natural process of repair has been described in many tissues and organs of the body. It is the natural process of tissue repair taking place in the body every day of our lives, from the day we are born!
Let’s briefly describe this process that takes place any time a tissue is exposed to stress and needs repair.
A few hours after an instance of tissue stress or damage, the affected tissue releases a compound called Granulocyte Colony-Stimulating Factor (G-CSF).25 G-CSF is well known to trigger stem cell release from the bone marrow. G-CSF is routinely used prior to cancer treatments involving chemotherapy or radiation.
Since such treatments are known to kill all stem cells in the body, requiring stem cell transplantation after the treatment, G-CSF is commonly injected into cancer patients to trigger stem cell release from the bone marrow in order to harvest and cryo-preserve stem cells.
After the treatment, the stem cells are thawed and re-injected in the patient to reconstitute the bone marrow. After tissue damage, as its concentration slowly and naturally increases in the blood, G-CSF triggers the release of stem cells from the bone marrow, increasing the number of stem cells circulating in the blood.25 Much scientific evidence indicates that this aspect is probably the most crucial part of the whole process. Increasing the number of circulating stem cells means that more stem cells are available to migrate in the damaged tissue.
Soon afterward, the affected tissue releases a unique compound called Stromal-Derived Factor-1 (SDF1).26 SDF-1 is the only compound known to attract stem cells.
When SDF-1 binds to CXCR4, a receptor present on the surface of stem cells, this binding process triggers the expression of adhesion molecules on the surface of the cell.
Therefore, as SDF-1 diffuses from the affected area to the blood circulation and as stem cells circulating in the blood travel through the affected tissue, the binding of SDF-1 to CXCR4 triggers the adhesion of stem cells to the capillary wall and subsequently their migration into the tissue.
When they arrive in the target tissue, stem cells proliferate and then differentiate into cells of that tissue, thereby assisting in the repair of the tissue.
This whole process has now been demonstrated in numerous studies and stem cells have been shown to participate to the repair of muscles, bone, pancreas, brain, skin, liver, intestine, lung … virtually every organ and tissue of the body!
In this whole process, the number of stem cells circulating in the bloodstream appears to be the most important factor. When the level of circulating stem cells was measured in the bloodstream of individuals who suffered an injury, the individuals who had the largest number of stem cells on the day of their injury showed the fastest and greatest recovery.
Likewise, when the number of stem cells was quantified in the bloodstream of nearly 500 individuals and their health condition was monitored for one year, the individuals with a larger number of stem cells in their blood showed a greater level of health.30 In other words, more stem cells circulating in the bloodstream means more stem cells available to migrate into tissues that might need assistance.
Safe Daily Stem Cell Support, A Novel Approach to Wellness All these discoveries surround the work I have done on a little known aquatic botanical called Aphanizomenon flos-aquae (AFA). AFA has been in the marketplace for nearly 3 decades and people consuming it have reported a wide variety of health benefits.
These benefits were initially classified into three broad categories: 1) benefits on the immune system, 2) anti-inflammatory properties, and 3) increase in mental clarity and a sense of mental energy.
Over the years, specific compounds were identified in AFA that partially explained the reported benefits.
1)AFA contains a polysaccharide that supports the activation of a specific type of lymphocyte called natural killer (NK) cells, as well as their migration out of the blood into tissues.
It is in the tissues that NK cells can carry out their specific task of scavenging and killing dysfunctional cells.
AFA was also shown to stimulate macrophage activity, macrophages being the first line of defense of the human body.32 2)AFA contains a blue pigment called phycocyanin. In the living AFA cell, phycocyanin acts as a powerful antioxidant.
But aside from its antioxidant properties, phycocyanin strongly supports a healthy inflammatory process.
3)AFA contains a unique compound called phenylethylamine (PEA). PEA is a natural compound produced by the brain when one is in love or content; in chemistry it is called the “molecule of love”. A deficiency in PEA has been associated with poor concentration, low mood and even at times depression, and oral consumption of PEA has been shown to alleviate these conditions.
The most common benefit reported by people consuming AFA is an increase in mental energy and clarity. Oral intake of PEA may also support a healthier sleep pattern.
But throughout the years, people also reported a wide range of health benefits touching various aspects of human physiology that could not be fully explained by the presence of these compounds.
How one single botanical product could produce so many benefits remained a mystery for many years, until the recent discovery that AFA contains a compound defined as an L-selectin ligand that triggers stem cell release from the bone marrow. L-selectin is an adhesion molecule that plays a critical role in the maintenance of stem cells in the bone marrow.
Blocking L-selectin increases the probability that a stem cell gets released from the bone marrow.40 We have developed a proprietary concentrate of AFA that concentrates the L-selectin ligand.
Feeding one gram of this AFA concentrate to individuals was shown to increase the number of circulating CD34+ stem cells and endothelial progenitor cells by 50% and 80%, respectively, a few hours after consumption. It is difficult to estimate exactly how many stem cells have been released, as many of the released stem cells also migrate in tissues. But considering the area under the curve, this corresponds to adding approximately 4-8 million new stem cells to the bloodstream.
While supporting the natural renewal system, such increase is well within normal physiological range of the body and presents no risk for the body.
After having developed and validated the method to quantify moderate fluctuations in the number of circulating stem cells, we then began to look at other plants that had been historically associated with a broad variety in health benefits, with the hypothesis that one of their mechanisms of action could be the mobilisation of bone marrow stem cells.
Through this work we have identified that fucoidan from the seaweed Undaria pinnatifida, also known in Japanese cuisine as wakame, works by increasing the baseline number of circulating stem cells over time.
An extract of echinacea was also shown to support stem cell release from the bone marrow.
Likewise, extracts of various species of aloe were shown to support hematopoiesis and increase the number of circulating stem cells. On the other hand specific extracts of (1,3)-(1,6)-beta-glucan have been shown to support the migration of stem cells into tissues.
Supporting the natural release of stem cells from the bone marrow provides for mild and safe daily support of stem cell physiology.
Supporting stem cell physiology is a new paradigm in health and wellness, and much scientific evidence indicates that this may very well be the best strategy to assist the body in maintaining optimal health.
STEM CELLS AND HEALTH
The discovery that increasing the number of circulating stem cells equates to greater health, coupled with the discovery of natural compounds that support the release of stem cells from the bone marrow and their migration into tissues, offers a new strategy in the pursuit of health and wellness. In theory, since BMSC have the ability of becoming virtually any cells of the body, supporting stem cell release and migration has the potential of supporting all aspects of human health.
BMSC have been shown to support the health of the nervous system, cardiac function, liver function, pancreatic function, kidney function, as well as lung, skin, and bone health.
In essence the discovery of the role of stem cells in the body leads to a broader understanding of how the body takes care of itself, opening exciting avenues in our quest for optimal health.
A New Paradigm The discovery that BMSC constitute the natural repair and renewal system of the body has paved the way to a new paradigm in health and wellness.
Once we understand that every day of our lives the role of stem cells is to patrol the body and migrate into areas needing assistance, then we realise that supporting stem cell physiology is the best strategy to maintain optimal health.
Health problems do not begin the day we receive a diagnosis or the day we suddenly decide that we have had enough, that quality of life has decreased to a level we are no longer willing to accept, at which point we decide to go and see the doctor… health problems begin to develop years if not decades before we experience the real problem.
As mentioned previously, the number of stem cells circulating in the bloodstream has been shown to be a determinant factor for overall health.
More stem cells circulating in the blood equates to greater health, as more stem cells are available for the day-to-day natural process of repair in the whole body.
Therefore, supporting the release of stem cells from the bone marrow and their migration into tissue on a daily basis constitutes one of the most promising ways of helping the body regain and maintain optimal health.
The discovery of the natural renewal system of the body, along with the discovery of natural products that support stem cell function, opens the door to a novel way of looking at health.
Instead of looking at health as an absence of illness and at any health-promoting strategy as a way to postpone illnesses, we can begin to look at health as a natural process, an intrinsic ability of the body.
The human body possesses the natural ability to remain healthy, and supporting this natural ability by increasing the number of circulating stem cells is logically the best way to enjoy optimal health.
COPYRIGHT © 2017 Christian Drapeau
We now have Dr Drapeaus STEMREGEN product available in our NZ store here
REFERENCES 1 Woodbury D, Schwarz EJ, Prockop DJ, and Black IB (2000) Adult Rat and Human Bone Marrow Stromal Cells Differentiate Into Neurons. J. Neurosci Res 61:364–370. 2 Sanchez-Ramos JR (2002) Neural Cells Derived From Adult Bone Marrow and Umbilical Cord Blood. J. Neurosci Res 69:880893. 3 Jang YY, Collector MI, Baylin SB, Diehl AM, and Sharkis SJ (2004) Hematopoietic stem cells convert into liver cells within days without fusion. Nature Cell Biol. 6(6):532-529. 4 Schwartz RE, Reyes M, Koodie L, Jiang Y, Blackstad M, Lund T, Lenvik T, Johnson S, Hu WS, and Verfaillie CM (2002) Multipotent adult progenitor cells from bone marrow differentiate into functional hepatocyte-like cells. J. Clin. Invest. 109:12911302. 5 Amoh, Y., Li, L., Katsuoka, K., and Hoffman, R.M. (2008) Multipotent hair follicle stem cells promote repair of spinal cord injury and recovery of walking function. Cell Cycle 7:1865-1869. 6 Goh ELK, Ma D, Ming GL, and Song H (2003) Adult Neural Stem Cells and Repair of the Adult Central Nervous System. J. Hematotherapy & Stem Cell Research 12:671-679 7 Efrat S. Generation of insulin-producing cells from stem cells for cell replacement therapy of type 1 diabetes. Isr Med Assoc J. 2004 May;6(5):265-7. 8 Kicic A, Shen WY, Wilson AS, Constable IJ, Robertson T, Rakoczy PE. Differentiation of marrow stromal cells into photoreceptors in the rat eye. J Neurosci. 2003 Aug 27;23(21):7742-9. 9 Orlic D., Kajstura J., Chimenti S. et al. Bone marrow cells regenerate infarcted myocardium. Nature 2001; 410(6829): 701–705. 10 Togel F and Westenfelder C (2007) Adult Bone Marrow–Derived Stem Cells for Organ Regeneration and Repair. Developmental Dynamics 236 (12):3321-31. 11 Bianco P, Riminucci M, Gronthos S, and Robey PG (2001) Bone Marrow Stromal Stem Cells: Nature, Biology, and Potential Applications. Stem Cells 19:180-192. 12 Wang X, Foster M, Al-Dhalimy M, Lagasse E, Finegold M, and Grompe M (2003) The origin and liver repopulating capacity of murine oval cells. PNAS 100(suppl.1):11881-11888. 13 Barker N, van de Wetering M, Clevers H. (2008) The intestinal stem cell. Genes Dev. 22(14):1856-64. 14 Kuang S, Gillespie MA, Rudnicki MA. (2008) Niche regulation of muscle satellite cell self-renewal and differentiation. Cell Stem Cell. 10;2(1):22-31. 15 Revishchin AV, Korochkin LI, Okhotin VE, Pavlova GV. (2008) Neural stem cells in the mammalian brain. Int Rev Cytol. 265:55109. 16 Burke ZD, Thowfeequ S, Peran M, Tosh D. (2007) Stem cells in the adult pancreas and liver. Biochem J. 404(2):169-78. 17 Díaz-Flores L Jr, Madrid JF, Gutiérrez R, Varela H, Valladares F, Alvarez-Argüelles H, Díaz-Flores L. (2006) Adult stem and transit-amplifying cell location. Histol Histopathol. 21(9):995-1027. 18 Abedi M, Greer DA, Colvin GA, Demers DA, Dooner MS, Harpel JA, Weier HU, Lambert JF, and Quesenberry PJ (2004) Robust conversion of marrow cells to skeletal muscle with formation of marrow-derived muscle colonies: A multifactorial process. Exp. Hematol. 32:426-434. 19 Fraser JK, Schreiber RE, Zuk PA, and Hedrick MH (2004) Adult stem cell therapy for the heart. Intern. J Biochem & Cell Biol 36:658–666 20 Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M, Kearne M, Magner M, and Isner JM (1999) Bone Marrow Origin of Endothelial Progenitor Cells Responsible for Postnatal Vasculogenesis in Physiological and Pathological Neovascularization. Circ Res. 85:221-228. 21 Krause DS, Theise ND, Collector MI, Henegariu O, Hwang S, Gardner R, Neutzel S, and Sharkis SJ (2001) Multi-organ, multilineage engraftment by a single bone marrow-derived stem cell. Cell 105:369-377 22 Branski LK, Gauglitz GG, Herndon DN, and Jeschke MG. (2008) A review of gene and stem cell therapy in cutaneous wound healing. Burns, July 4. 23 Dezawa M, Ishikawa H, Hoshino M, Itokazu Y, and Nabeshima Y. (2005) Potential of bone marrow stromal cells in applications for neuro-degenerative, neuro-traumatic and muscle degenerative diseases. Curr Neuropharmacol. 3(4):257-66. 24 Jensen GS, Drapeau C. (2002) The use of in situ bone marrow stem cells for the treatment of various degenerative diseases. Med Hypotheses. 59(4):422-8. 25 Leone AM, Rutella S, Bonanno G, Contemi AM, de Ritis DG, Giannico MB, Rebuzzi AG, Leone G, Crea F. (2006) Endogenous GCSF and CD34+ cell mobilization after acute myocardial infarction. Int J Cardiol. 111(2):202-8. 26 Abbott JD, Huang Y, Liu D, Hickey R, Krause DS, Giordano FJ. (2004) Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation 110(21):3300-5. 27 Peled A, Grabovsky V, Habler L, Sandbank J, Arenzana-Seisdedos F, Petit I, Ben-Hur H, Lapidot T, Alon R. (1999) The chemokine SDF-1 stimulates integrin-mediated arrest of CD34(+) cells on vascular endothelium under shear flow. J Clin Invest. 104(9):1199211. 28 Vandervelde S, van Luyn MJ, Tio RA, Harmsen MC. (2005) Signaling factors in stem cell-mediated repair of infarcted myocardium. J Mol Cell Cardiol. 39(2):363-76. 29 Tomoda H, Aoki N. (2003) Bone marrow stimulation and left ventricular function in acute myocardial infarction. Clin Cardiol. 26(10):455-7. 30 Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, Böhm M, Nickenig G. (2005) Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 353(10):999-1007. 31 Jensen GS, Ginsberg DI, Huerta P, Citton M, and Drapeau C. (2000) Consumption of Aphanizomenon flos-aquae has rapid effects on the circulation and function of immune cells in humans. JANA 2(3):50-58. 32 Pugh N and Pasco DS. (2001) Characterization of human monocyte activation by a water soluble preparation of Aphanizomenon flos-aquae. Phytomedicine 8(6):445-53. 33 Hart A, Zaske LA, Patterson KM, Drapeau C, and Jensen GS (2007) Natural Killer Cell Activation and Modulation of Chemokine Receptor Profile. In Vitro by an Extract from the Cyanophyta Aphanizomenon flos-aquae. J Med Food 10(3): 435–441 34 Benedetti S, Benvenuti F, Pagliarani S, Francogli S, Scoglio S, Canestrari F. (2004) Antioxidant properties of a novel phycocyanin extract from the blue-green alga Aphanizomenon flos-aquae. Life Sciences75(19):2353-2362. 35 Reddy CM, Bhat VB, Kiranmai G, Reddy MN, Reddanna P, Madyastha KM (2000) Selective inhibition of cyclooxygenase-2 by Cphycocyanin, a biliprotein from Spirulina platensis. Biochem Biophys Res Commun 277(3): 599-603. 36 Romay C, Ledon N, and Gonzalez R. (1999) Phycocyanin extract reduces leukotriene B4 levels in arachidonic acid-induced mouseear inflammation test. J Pharm Pharmacol 51(5):641-642. 37 Sandler M, Ruthven CR, Goodwin BL, Coppen A. (1979) Decreased cerebrospinal fluid concentration of free phenylacetic acid in depressive illness. Clin Chim Acta 93(1):169-71 38 Baker et al. (1991) Phenylethylaminergic mechanisms in attention-deficit disorder. Biol Psychiatry 1991 Jan 1;29(1):15-22 39 Frenette PS and Weiss L. Sulfated glycans induce rapid hematopoietic progenitor cell mobilization: evidence for selectin-dependent and independent mechanisms. Blood, Vol 96, No 7, pp. 2460-8, 2000 40 Cottler-Fox MH, Lapidot T, Petit I, Kollet O, DiPersio JF, Link D, Devine S. (2003) Stem cell mobilization. Hematology Am Soc Hematol Educ Program. 419-437. 41 Jensen GS, Hart AN, Zaske LAM, Drapeau C, Schaeffer DJ and Cruickshank JA. (2007) Mobilization of human CD34+CD133+ and CD34+CD133- stem cells in vivo by consumption of an extract from Aphanizomenon flos-aquae - related to modulation of CXCR4 expression by an L-selectin ligand. Cardiovascular Revascularization Medicine, 8(3):189-202. 42 Irhimeh MR, Fitton JH, Lowenthal RM. (2007) Fucoidan ingestion increases the expression of CXCR4 on human CD34+ cells. Exp Hematol. 2007 Jun;35(6):989-94. 43 Abdelmonem M, Kassem SH, Gabr H, Shaheen AA, Aboushousha T. (2015) Avemar and Echinacea extracts enhance mobilization and homing of CD34(+) stem cells in rats with acute myocardial infarction. Stem Cell Res Ther. 2015 Sep 14;6:172. 44 Egger SF, Brown GS, Kelsey LS, Yates KM, Rosenberg LJ, Talmadge JE. (1996) Studies on optimal dose and administration schedule of a hematopoietic stimulatory beta-(1,4)-linked mannan. Int J Immunopharmacol. 1996 Feb;18(2):113-26. 45 Egger SF, Brown GS, Kelsey LS, Yates KM, Rosenberg LJ, Talmadge JE. (1996) Hematopoietic augmentation by a b-(1,4)-linked mannan. Cancer Immunol Immunother (1996) 43:195 –205. 46 Drapeau C, Benson BF, James J, and Jensen GS. (2015) Aloe macroclada from Madagascar Triggers Transient Bone Marrow Stem Cell Mobilization. J Stem Cell Res Ther. Vol 5(6). 47 Woo YI, Park BJ, Kim HL, Lee MH, Kim J, Yang YI, Kim JK, Tsubaki K, Han DW, Park JC. (2010) The biological activities of (1,3)-(1,6)-beta-d-glucan and porous electrospun PLGA membranes containing beta-glucan in human dermal fibroblasts and adipose tissue-derived stem cells. Biomed Mater. 2010 Aug;5(4):044109. 48 Zhao M, Momma S, Delfani K, Carlen M, Cassidy RM, Johansson CB, Brismar H, Shupliakov O, Frisen J, Janson AM. (2003) Evidence for neurogenesis in the adult mammalian substantia nigra. PNAS 100(13):7925-30. 49 Carreras E, Saiz A, Marín P, Martínez C, Rovira M, Villamor N, Aymerich M, Lozano M, Fernández-Avilés F, Urbano-Izpizua A, Montserrat E, Graus F. (2003) CD34+ selected autologous peripheral blood stem cell transplantation for multiple sclerosis: report of toxicity and treatment results at one year of follow-up in 15 patients. Haematologica 88(3):306-14. 50 Ferrari G, Cusella-De Angelis G, Coletta M, Paolucci E, Stornaiuolo A, Cossu G, Mavilio F. (1998) Muscle regeneration by bone marrow-derived myogenic progenitors. Science 279(5356):1528-30. 51 Tomita M, Adachi Y, Yamada H, Takahashi K, Kiuchi K, Oyaizu H, Ikebukuro K, Kaneda H, Matsumura M, Ikehara S. (2002) Bone marrow-derived stem cells can differentiate into retinal cells in injured rat retina. Stem Cells 20(4):279-83. 52 Kawada H, Takizawa S, Takanashi T, Morita Y, Fujita J, Fukuda K, Takagi S, Okano H, Ando K, Hotta T. (2006) Administration of hematopoietic cytokines in the subacute phase after cerebral infarction is effective for functional recovery facilitating proliferation of intrinsic neural stem/progenitor cells and transition of bone marrow-derived neuronal cells. Circulation 113(5):70110. 53 Ince H, Petzsch M, Kleine HD, Schmidt H, Rehders T, Körber T, Schümichen C, Freund M, Nienaber CA. (2005) Preservation from left ventricular remodeling by front-integrated revascularization and stem cell liberation in evolving acute myocardial infarction by use of granulocyte-colony-stimulating factor (FIRSTLINE-AMI). Circulation 112(20):3097-106. 54 Orlic D, Hill JM, Arai AE. (2002) Stem cells for myocardial regeneration. Circ Res. 91(12):1092-102. 55 Orlic D, Kajstura J, Chimenti S, Limana F, Jakoniuk I, Quaini F, Nadal-Ginard B, Bodine DM, Leri A, Anversa P. (2001) Mobilized bone marrow cells repair the infarcted heart, improving function and survival. PNAS 98(18):10344-9. 56 Kollet O, Shivtiel S, Chen YQ, Suriawinata J, Thung SN, Dabeva MD, Kahn J, Spiegel A, Dar A, Samira S, Goichberg P, Kalinkovich A, Arenzana-Seisdedos F, Nagler A, Hardan I, Revel M, Shafritz DA, Lapidot T. (2003) HGF, SDF-1, and MMP-9 are involved in stress-induced human CD34+ stem cell recruitment to the liver. J Clin Invest. 112(2):160-9. 57 Sun Y, Chen L, Hou XG, Hou WK, Dong JJ, Sun L, Tang KX, Wang B, Song J, Li H, Wang KX. (2007) Differentiation of bone marrow-derived mesenchymal stem cells from diabetic patients into insulin-producing cells in vitro. Chin Med J (Engl) 120(9):7716. 58 Ianus A, Holz GG, Theise ND, Hussain MA. (2003) In vivo derivation of glucose-competent pancreatic endocrine cells from bone marrow without evidence of cell fusion. J Clin Invest. 111(6):843-50. 59 Lee RH, Seo MJ, Reger RL, Spees JL, Pulin AA, Olson SD, Prockop DJ. (2006) Multipotent stromal cells from human marrow home to and promote repair of pancreatic islets and renal glomeruli in diabetic NOD/scid mice. PNAS 103(46):17438-43. 60 Herrera MB, Bussolati B, Bruno S, Fonsato V, Romanazzi GM, Camussi G. (2004) Mesenchymal stem cells contribute to the renal repair of acute tubular epithelial injury. Int J Mol Med. 14(6):1035-41. 61 Iwasaki M, Adachi Y, Minamino K, Suzuki Y, Zhang Y, Okigaki M, Nakano K, Koike Y, Wang J, Mukaide H, Taketani S, Mori Y, Takahashi H, Iwasaka T, Ikehara S. (2005) Mobilization of bone marrow cells by G-CSF rescues mice from cisplatin-induced renal failure, and M-CSF enhances the effects of G-CSF. J Am Soc Nephrol. 16(3):658-66. 62 Rojas M, Xu J, Woods CR, Mora AL, Spears W, Roman J, Brigham KL. (2005) Bone marrow-derived mesenchymal stem cells in repair of the injured lung. Am J Respir Cell Mol Biol. 33(2):145-52. 63 Yamada M, Kubo H, Kobayashi S, Ishizawa K, Numasaki M, Ueda S, Suzuki T, Sasaki H. (2004) Bone marrow-derived progenitor cells are important for lung repair after lipopolysaccharide-induced lung injury. J Immunol. 172(2):1266-72. 64 Mansilla E, Marín GH, Drago H, Sturla F, Salas E, Gardiner C, Bossi S, Lamonega R, Guzmán A, Nuñez A, Gil MA, Piccinelli G, Ibar R, Soratti C. (2006) Bloodstream cells phenotypically identical to human mesenchymal bone marrow stem cells circulate in large amounts under the influence of acute large skin damage: new evidence for their use in regenerative medicine. Transplant Proc. 38(3):967-9. 65 Borue X, Lee S, Grove J, Herzog EL, Harris R, Diflo T, Glusac E, Hyman K, Theise ND, Krause DS. (2004) Bone marrow-derived cells contribute to epithelial engraftment during wound healing. Am J Pathol. 165(5):1767-72. 66 Bozlar M, Aslan B, Kalaci A, Baktiroglu L, Yanat AN, Tasci A. (2005) Effects of human granulocyte-colony stimulating factor on fracture healing in rats. Saudi Med J. 26(8):1250-4. 67 Burt RK, Oyama Y, Verda L, Quigley K, Brush M, Yaung K, Statkute L, Traynor A, Barr WG. (2004) Induction of remission of severe and refractory rheumatoid arthritis by alloge